Jointly is a cannabis wellness app that launched in April 2020. Jointly’s mission is to help people discover purposeful cannabis consumption. Purposeful cannabis consumption starts with the question: why do you use cannabis?
Many people use cannabis or CBD to manage their chronic pain. What does it look like to use cannabis or CBD to manage pain?
It could be a young woman who finds that a few puffs from a high THC vape pen at the onset of her migraines dramatically decreases her symptoms; or a hard-charging dad who uses CBD capsules to soothe his inflamed joints after a weekend of hiking with his grown children; or a cancer survivor with lingering nerve pain from chemotherapy who traded prescription opiates for a few puffs from a joint on the recommendation of her doctor.
Is Cannabis Good for Pain Relief?
Cannabis has been used to soothe pain for at least 5000 years. While cannabis may not be a mainstream pain reliever anymore, the majority of medical marijuana patients use cannabis to manage their chronic pain. Many feel it is highly effective.
For example, a 2019 survey of medical cannabis patients found that 65% of patients reported taking cannabis to relieve pain, and of that group, 80% reported that cannabis was “very or extremely helpful” for managing their pain.
A separate study conducted on 2987 people reporting their cannabis use and symptom relief found that cannabis benefitted numerous pain conditions including non-specified pain, headaches, back, muscle or joint pain, and gastrointestinal pain. These researchers noted that whole cannabis flower was associated with greater pain relief than any other type of product, and that higher THC levels were “the strongest predictors of analgesia.” Interestingly, CBD levels “were not associated with pain relief.”
Clearly, people feel that cannabis helps them manage their pain, but these data come from self-reported studies rather than clinical studies. What do clinical studies indicate about cannabis and pain?
What Does the Science Say About Cannabis and Pain?
The scientific literature holds seemingly contradictory findings. For example, despite the survey results above, many clinical studies indicate that cannabinoids have only weak analgesic properties.
A 2018 editorial published in the Journal of Applied Laboratory Medicine (JALM) states, “systematic reviews in acute pain are unequivocal in pointing out the lack of effectiveness of cannabinoids,” and “the reviews in chronic pain, mostly neuropathic, have arrived at similar conclusions, that cannabinoids and medical cannabis provide small analgesic benefit.”
How is it possible that people feel cannabis is highly effective at managing their pain, but clinical trials indicate that cannabinoids and cannabis are weak or ineffective analgesics?
Limitations of Cannabis Research
Decades of prohibition have created a situation where there simply aren’t many scientifically rigorous studies on cannabis and pain. As a result, “the current clinical debate continues to be driven, in large part, by variable analyses and perspectives of the same extant clinical trials.”
However, prohibition is only a piece of the puzzle. Many of the studies that found minimal benefit for pain used synthetic cannabinoids. Modern medicine and pharmacology follow a standard path of developing “safer and more efficacious drugs than plants themselves.”
However, there is evidence that isolated cannabinoids and synthetic cannabinoids may have less therapeutic benefit than the whole plant. For example, a 2018 review published in Pharmacotherapy states, “surprisingly, and as an unforeseen paradox to modern pharmacy…oral pharmaceutical grade cannabinoids show conflicting results in patients with chronic pain.” The authors of the review note that the evidence indicates that “oral cannabinoids are inferior when compared to…the cannabis plant.”
The editorial in JALM concedes, “it may be presumptuous to conclude that the major clinical effects of cannabis are derived solely from THC and cannabidiol (CBD). What becomes lost in the rhetoric…[is] the putative analgesic effects of terpenes and flavonoids.”
Beyond terpenes and flavonoids, there may be lesser-known cannabinoids in the whole cannabis plant that contribute to its pain-relieving effects. For example, a September 2020 article published in the medical journal Comprehensive Clinical Medicine notes that there are “hundreds of cannabinoid compounds…in the cannabis plant that variably activate CB1 and CB2 receptors.”
Part of the reason why clinical studies produce mixed results seems to be that these studies use isolated or synthetic cannabinoids, which seem to have less therapeutic benefit than the whole plant. In line with this idea, many surveys and self-reported studies indicate that cannabis flower is more effective than other types of products for relieving pain.
Supporting this notion, the National Academy of Sciences, Engineering, and Medicine found “substantial evidence that inhaled cannabis is effective for the treatment of chronic pain in adults.”
What Type of Pain Does Cannabis Help With?
There are three main pain systems: nociceptive pain, neuropathic pain, and central pain.
When your tissue is inflamed or injured, special pain detecting neurons called nociceptors transmit this information “via nociceptive pathways in the spinal cord to the brain.” Your brain interprets these signals and creates the subjective experience of pain.
In nociceptive pain, the nervous system is functioning normally and noxious stimuli like disease, inflammation or injury activate the nociceptors, “leading to organized responses that defend the tissue under threat and aid in its repair.”
Neuropathic pain is caused by “damage to sensory or spinal nerves, which send inaccurate pain messages to higher centers.” Neuropathic pain is characterized by spontaneous pain, allodynia (pain from normally innocuous stimuli), and hyperalgesia (excessive pain from something that would normally be mildly painful).
Central pain can be nociceptive or neuropathic, but it is caused by “dysfunction that specifically affects the central nervous system, which includes the brain, brainstem and spinal cord.” Fibromyalgia is the classic example of central pain. Basically, the central nervous system amplifies the pain signal, making the pain impossible to ignore.
Pain researchers discovered that in some circumstances, acute pain can lead to “hyperexcitability” of the nociceptors, essentially lowering the threshold needed to activate these pain neurons. This plasticity is unique: “unlike other sensory systems, nociceptive systems can sometimes undergo very long lasting, even permanent, enhancement of function following sufficiently intense activation.”
This process leads to “amplification of incoming [pain] signals,” and is a substantial part of neuropathic and chronic pain conditions. These chronic pain conditions are difficult to treat, but there is evidence that cannabis is effective for managing these types of pain.
A 2019 review of cannabis and pain found that oromucosal sprays are effective in reducing chronic and neuropathic pain caused by cancer, that inhaled cannabis flower is effective in reducing neuropathic pain in general, and that oral cannabis is effective for nociceptive pain.
Your Brain Creates Pain
During World War II, H.K. Beecher, a physician serving with the U.S. Army, observed that nearly three-quarters of severely wounded soldiers were “alert, responsive and not in shock…reported no to moderate pain [and] did not want pain relief medication.” Beecher’s observations were the first indication that the body has natural mechanisms of modulating pain, which we now know can either diminish or magnify pain.
Pain modulation refers to the process by which “the body alters a pain signal as it is transmitted along the pain pathway.” This innate pain modulation is an important part of how cannabis helps people manage pain. While endorphins (the body’s endogenous opioids) are known to play a role in pain modulation, preclinical studies have revealed that the endocannabinoid system plays an important role as well.
For example, when researchers injected rats with naloxone, an opioid receptor antagonist that blocks the effects of opioids, alongside a synthetic cannabinoid that exerts similar effects to THC, they observed effects “analogous to the effect of morphine, but these effects were not blocked by naloxone, indicating that these effects are mediated specifically through cannabinoid receptors.”
How Does the Endocannabinoid System Modulate Pain?
After an injury, the body produces endocannabinoids that reduce inflammation and pain signaling at the site of injury, which reduces pain.
As Kevin Hill, MD et al. write in their 2017 clinical review of cannabis and pain, “understanding the function of endogenous cannabinoids helps explain the efficacy of exogenous cannabinoids…in treating pain.”
The endocannabinoid system is made up of the CB1 (cannabinoid receptor 1) and CB2 receptors and the endogenous cannabinoids (anandamide and 2-AG) that bind to them. The CB1 receptors are found in the brain, nervous system, peripheral organs and tissue, while the CB2 receptors are found primarily on immune cells, although they are also found on bone, spleen and liver cells.
Research has shown that the endocannabinoid system “acts independently of the opioid pathway to control pain signaling, immune activation, and inflammation.” Scientists have found that CB1 receptors are “found in high concentrations in areas of the brain that modulate nociceptive processing, with a similar distribution to opioid receptors.”
There is evidence that both CB1 and CB2 receptors play a role in cannabinoid pain relief, but the CB1 receptor is thought to have the most direct influence on pain processing pathways.
How Does Cannabis Relieve Pain?
Both cannabinoids and opioids relieve pain through a mechanism that “blocks the release of pain-propagating neurotransmitters in the brain and spinal cord.” Activating the cannabinoid receptors “by endogenous or extraneously administered cannabinoids” inhibits pain signals and neurotransmitter release locally, at the spinal level and at the supraspinal level.
As Kevin Hill, MD et al. write in their clinical review, due to the complex ways that the endocannabinoid system modulates pain, “the biologically hypothesized rationale for cannabinoid administration is whole-body exposure to exogenous cannabinoids to turn on pain inhibition.”
There is also evidence that when the endocannabinoid system is activated, it downregulates neuronal hyperexcitability. If you recall, this hyperexcitability of neurons is a primary factor involved in the development and maintenance of chronic pain and neuropathy.
How Does CBD Relieve Pain?
There are a variety of mechanisms by which CBD can help people manage pain. While CBD doesn’t bind to cannabinoid receptors, it does increase the levels of anandamide, the endocannabinoid that binds to CB1 receptors (like THC). As established, the CB1 receptors play an important role in pain modulation.
However, the effects of CBD on chronic pain “are likely due to modulation of multiple non-endocannabinoid signaling systems.”
For example, CBD “enhances the activity of [GABA] receptors,” which can dampen pain signals as they enter your brain. CBD is also “a potent antioxidant.”
Additionally, “the pharmacodynamic profile of CBD resembles those of many currently prescribed treatments for neuropathic pain,” and research has demonstrated that CBD has a marked anti-inflammatory effect in animals and in in vitro experiments. At present, the research into how CBD affects inflammation in humans is “limited and inconclusive.”
Cannabis Makes Pain More Tolerable?
Many factors can affect how pain is experienced: your emotional state, your degree of anxiety, whether you are distracted or focused on the pain, your expectations about the pain, etc.
Experimental studies on cannabis and pain indicate that cannabis increases the threshold at which participants feel pain, and decreases the unpleasantness of pain, but does not reduce the intensity of pain.
A separate study drew the conclusion that cannabis affected only one of three subjective measures of pain: bothersomeness. The other two measures were pain intensity and a McGill Pain Questionnaire.
These findings are important in understanding why cannabis is such an effective tool for managing pain. While cannabis may not decrease the intensity of pain in the same way opioids do, it makes pain more tolerable — and also does not seem to increase sensitivity to pain in the way opioids do.
Cannabis has the ability to affect “the emotional component of pain” by boosting mood, reducing symptoms of anxiety or depression, and “offering some degree of dissociation from physical symptoms.”
According to the biopsychosocial model, pain is not simply a biological process, but one that involves a person’s psychology and larger social network. If pain is less bothersome, it may be psychologically easier to tolerate and have less of a negative impact on well-being. Please note this information is for educational purposes only, and any changes to your pain management strategy should be discussed with your doctor.
Curious if cannabis or CBD can help you manage pain?
Use Jointly to Manage Pain with Cannabis and CBD
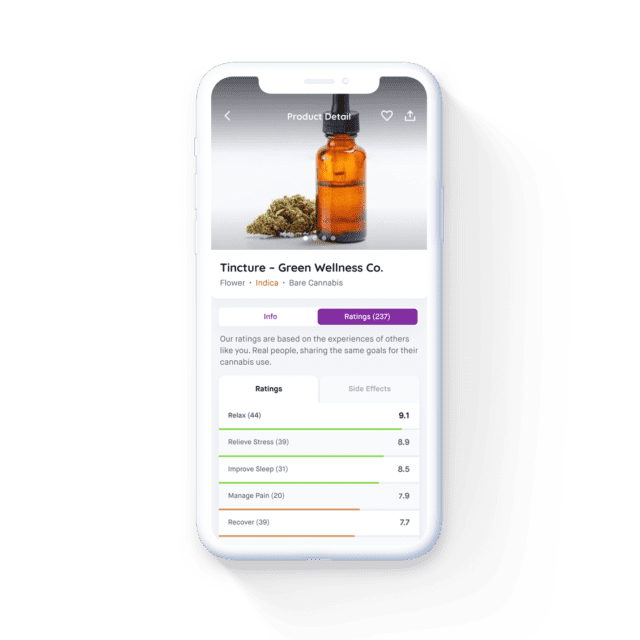
With Jointly, you measure how well a cannabis product helps you achieve your wellness goals, including pain management.
As you record how well a product helps you manage your pain, Jointly helps you track the 15 factors that can impact your results so that you can enjoy your ideal experience every time and minimize any side effects.
Jointly users who have optimized their cannabis consumption by reporting at least 10 cannabis sessions are feeling 38% better.
Download the Jointly app today and start accomplishing your wellness goals with cannabis and CBD!
Medical Disclaimer:
The information provided in these blog posts is intended for general informational and educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. The use of any information provided in these blog posts is solely at your own risk. The authors and the website do not recommend or endorse any specific products, treatments, or procedures mentioned. Reliance on any information in these blog posts is solely at your own discretion.






